Spinal Cord Tumor
Spinal Cord Tumor
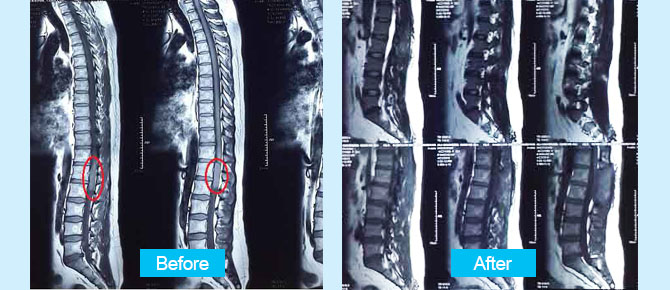
A 35-year-old man with numbness in his hip and weakness in lower limbs was referred to Dr. Sharifi. He diagnosed with spinal cord tumor. The patient was operated by Dr. Guive Sharifi in Erfan hospital.
He feels well after surgery, he has not experienced any disorder in his movement after operation and his pathology report is benign.
Preoperative Imaging:




Postoperative Imaging: