Lumbar disk disease
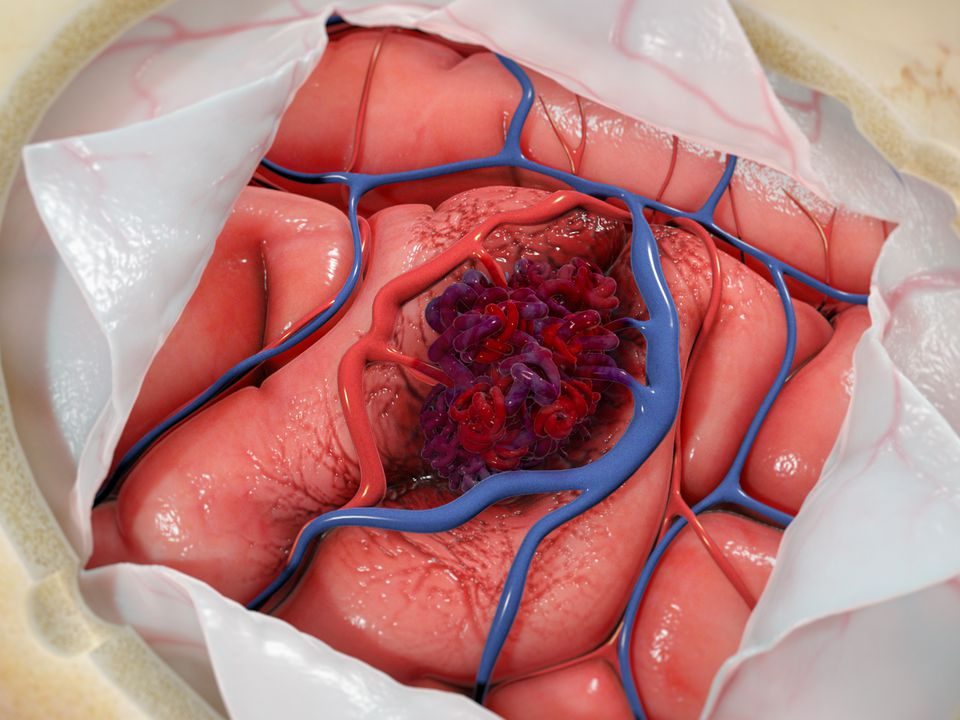
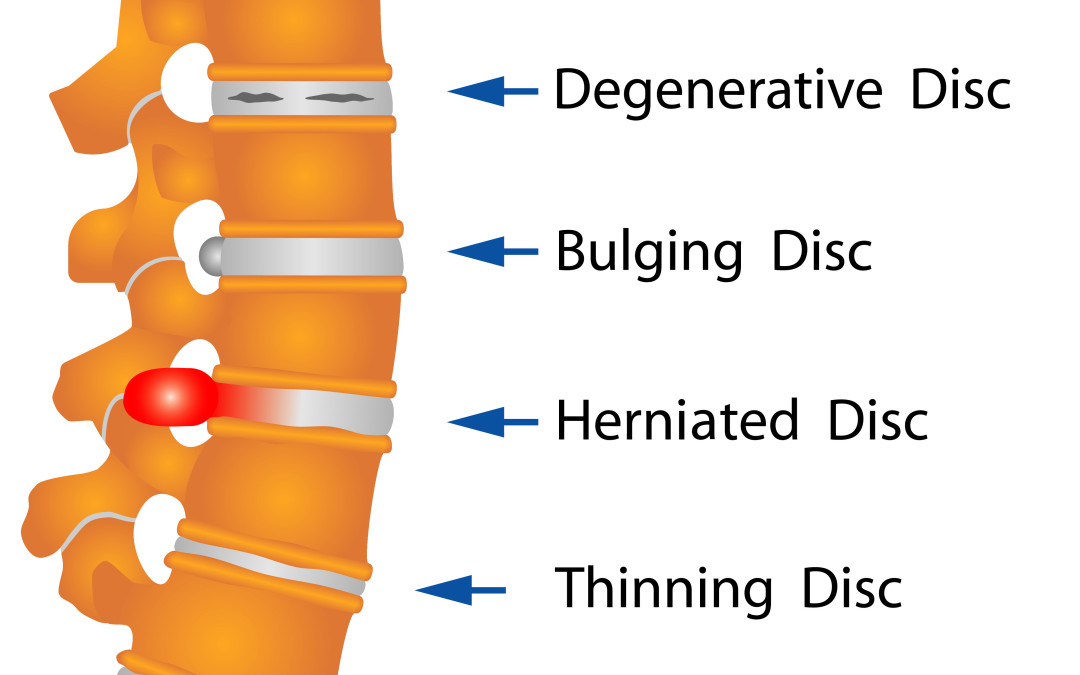
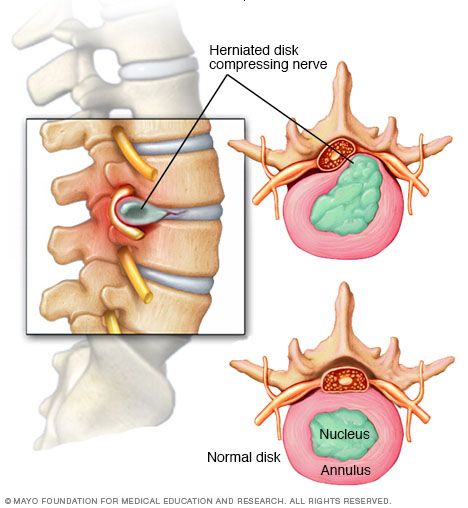
The human lumbar spine, like the entire spine, is an engineering marvel, uniquely evolved to support upright posture and permit a wide variety of movements. Crucial to these functions are the thin, compressible, fibrocartilaginous intervertebral disks. With age, the disks undergo progressive degenerative changes that affect their ability to subserve these roles. In certain circumstances, disk damage may accelerate these changes, drastically altering the load-bearing characteristics of the disk and leading to significant disk degeneration. In severe cases, this degeneration can be associated with considerable morbidity, including debilitating pain and neurological symptoms. the most common complaint of patients with disk disease is low back pain, often radiating to the sacroiliac joints. The pain is often vague, described as “deep” pain that is exacerbated by positions and activities such as spine flexion, standing, and sitting. Patients who have experienced protrusion or herniation of the nucleus as a result of degenerative disk disease may develop symptoms of nerve root compression or, in rare cases, of neurogenic claudication. These patients may experience symptoms associated with nerve root compression, including dermatomal sciatic pain, distal paresthesias, and myotomal motor weakness.
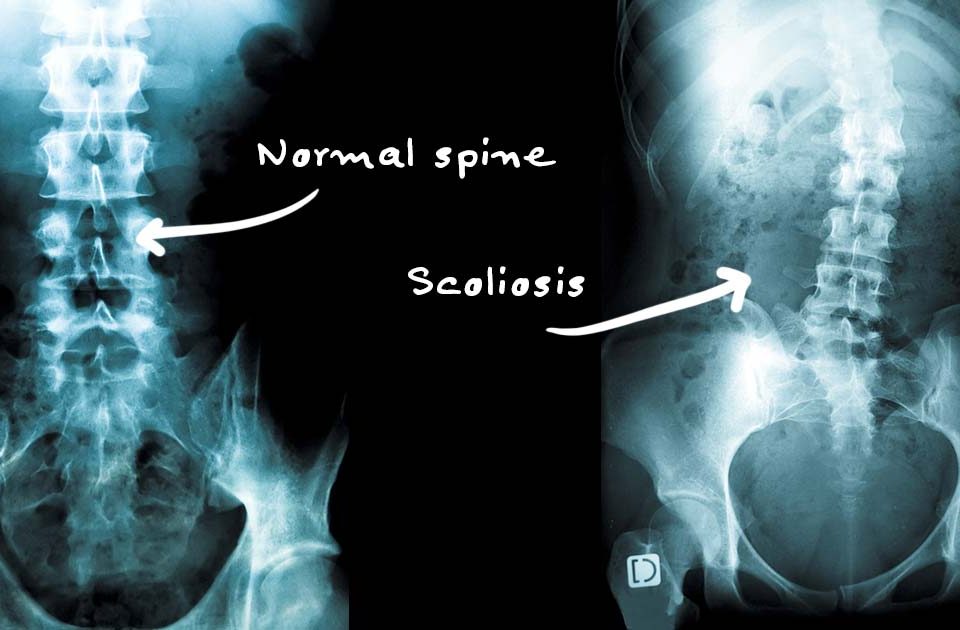
MRI is the preferred modality for evaluating the lumbar intervertebral disk, owing to its superior soft tissue resolution. Patients whose symptoms persist or progress over 4 to 6 weeks, or who exhibit concerning symptoms or history, should be imaged with MRI.
The initial management of acute low back pain, including that resulting from lumbar disk disease, is generally nonsurgical. the mainstays of therapy are reassurance and patient education, activity modification to limit disk loading, nonsteroidal anti-inflammatory drugs (NSAIDs) and/or acetaminophen, and a gradual return to physical activity. For those patients with prolonged symptoms, however, or in whom pain and neurological symptoms are progressive or particularly debilitating, surgical intervention may be contemplated. In general, the following principles for patient selection may be derived from the
foregoing:
(1) patients should be symptomatic; (2) their symptoms should correspond to findings on examination and imaging, and vice versa; (3) symptoms should be refractory to an extended course of appropriate nonsurgical management (5-8 weeks); (4) neurological deficit is indication for urgent surgery (5) there should be the reasonable expectation that surgery will improve their symptoms and functional status; and (6) the expected degree of improvement should justify the risks of surgical complications.